You may have heard there are racial disparities within the medical field—particularly among mothers. Unfortunately, African-American women and other racial minority mothers are far more likely to experience complications related to pregnancy and childbirth than their white peers.
Pregnancy-Related Mortality Ratios (PRMR) refer to the number of women who lose their lives as a result of pregnancy-related issues.
If you aren’t familiar with this subject, you may be surprised to learn that not all mothers are treated equally in hospitals. Similarly, the PRMR varies from state to state, which implies that mothers’ healthcare is not the same across the United States.
Here’s what you should know about PRMR:
There Are Disparities Across All Categories
According to the Centers for Disease Control and Prevention (CDC), about 700 women lose their lives in the United States each year due to pregnancy or its complications, and there are significant racial/ethnic disparities.
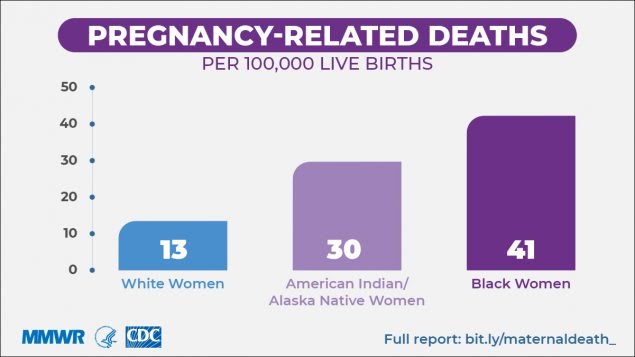
As you can see from the chart above, black women in the U.S. are three times more likely to die during pregnancy or childbirth than their white peers across all three categories:
- Location
- Age
- Education level
Location
The CDC analyzed the PRMR in every state throughout the country. They were then able to split state PRMR equally into three groups:
- High
- Medium
- Low
According to the data, “Even in states with the lowest PRMR, the PRMR for black women was about three times as high as the PRMR for white women.”
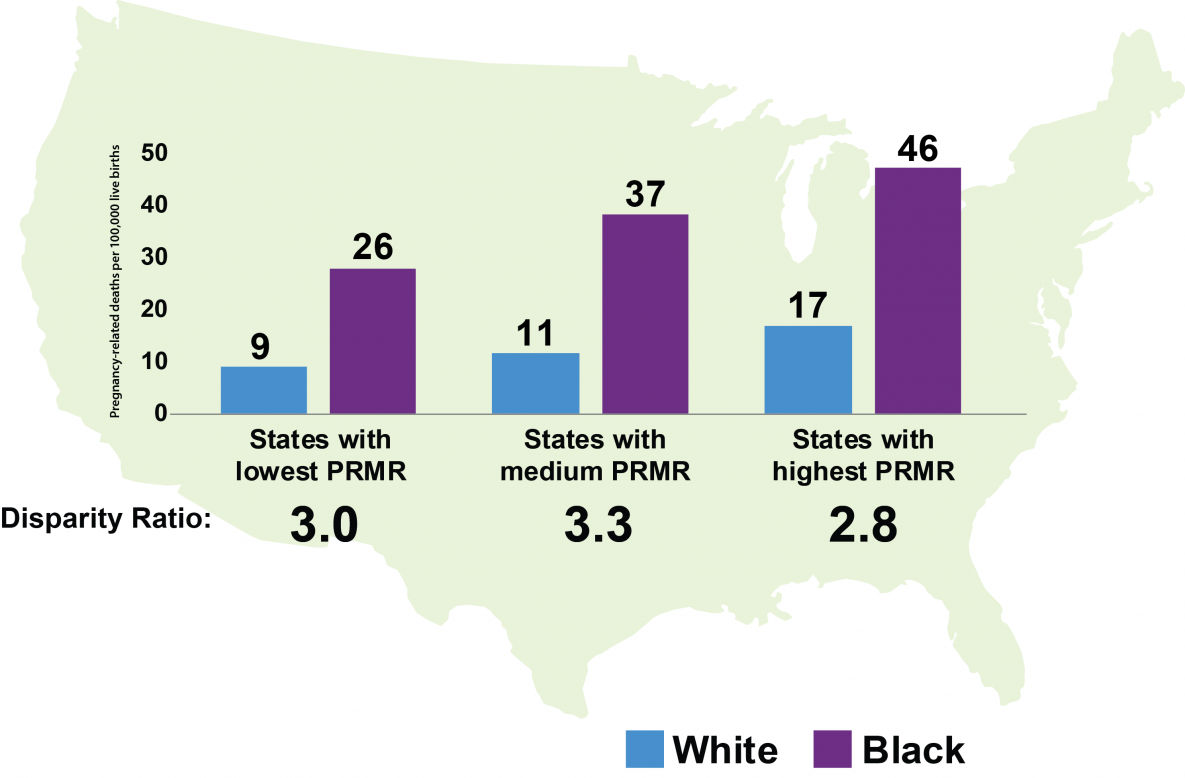
As you can see from the graph above, the disparity persists across all 50 states.
Age
As women age, pregnancy-related racial inequities increase. According to the CDC, “The disparity for black and American Indian/Alaskan Native women older than 30 years [are] four to five times [more likely to die as a result of childbirth] than their white counterparts. For example, the disparity ratio for black women compared to white women ranged from 1.5 among the <20 years age group to 4.3 for the 30-34 years age group.”
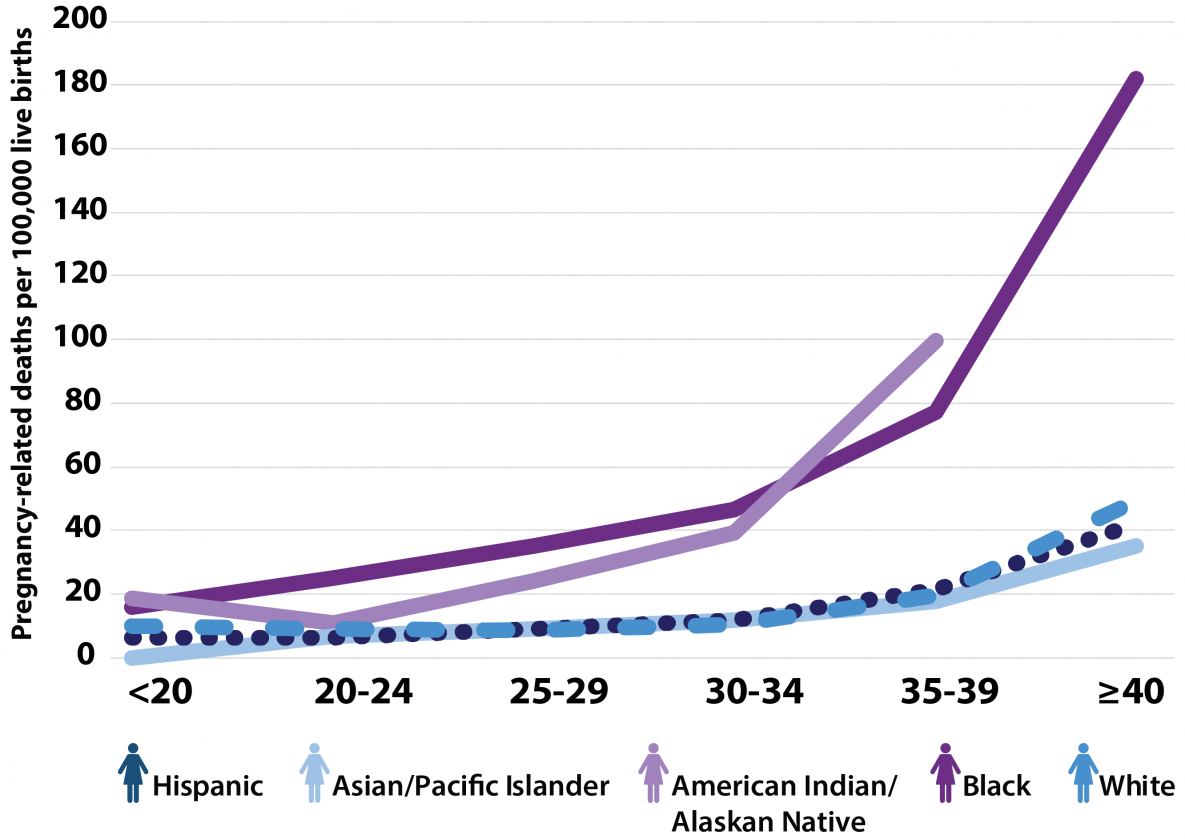
As you can see from the graph above, white, Asian/Pacific Islander, and Hispanic women are the least likely to experience fatal complications due to childbirth.
Education Level
Regardless of education level, black women are almost always the most likely to lose their lives as a result of pregnancy-related complications.
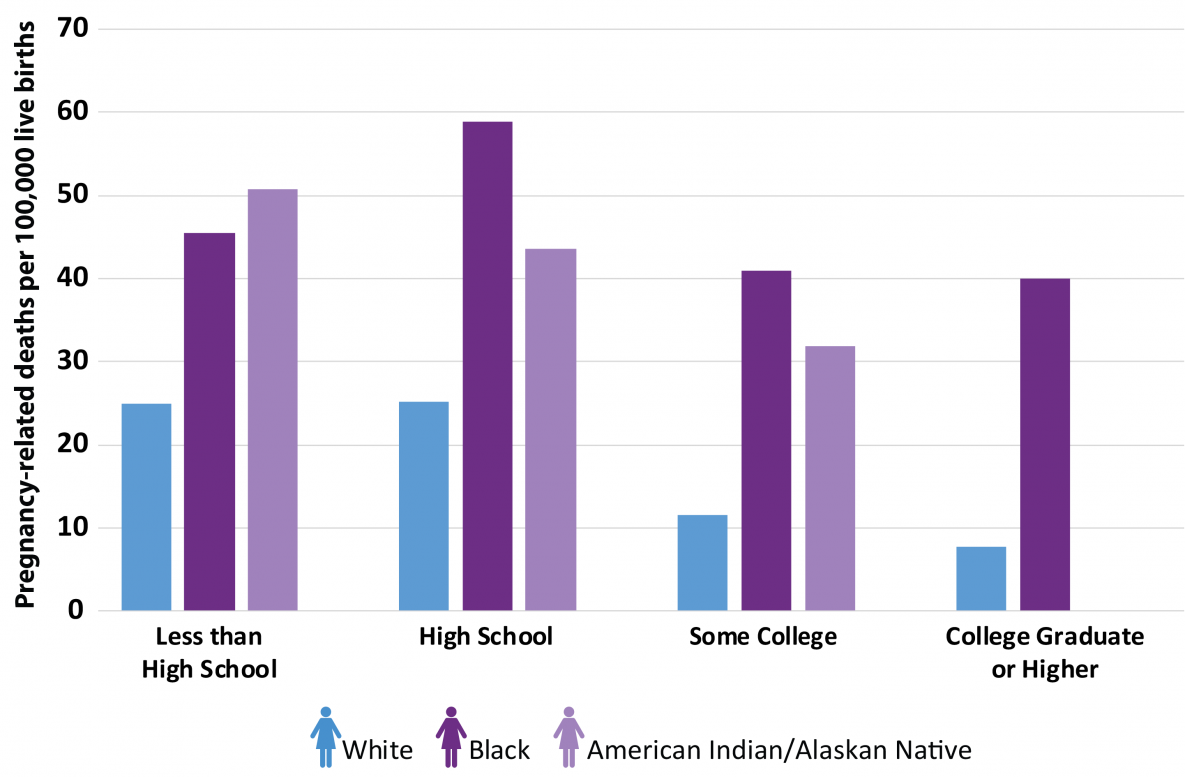
As you can see from the graph, the only group to surpass the black mother mortality rate is the American Indian/Alaskan Native group with less than a high school education.
What’s most alarming about this data is that black women with college degrees are more than three times as likely to die from pregnancy-related problems than their white counterparts.
The Issue Persists
Issues related to PRMR have persisted over the years. Over time, black women have consistently had the highest pregnancy-related mortality rates. The most common complications that occur are as follows:
- Hemorrhage
- Infection
- Amniotic fluid embolism
- Thrombotic pulmonary or another embolism
- Hypertensive disorders of pregnancy
- Anesthesia complications
- Cerebrovascular accidents
- Cardiomyopathy
- Other cardiovascular conditions
- Other noncardiovascular medical conditions
Reasons for PRMR
Genetics and education levels have a low impact on disparities regarding preterm birth. Studies show that air pollution is connected to spontaneous preterm birth, which Black women are more likely to be exposed to. Unfortunately, black women are four times as likely as white women to live in neighborhoods with high violent crime and high air pollution rates.
Similarly, systemic discrimination results in income inequality and residential segregation, which further impacts PRMR rates. Pregnancy-related health concerns can result from both physical and psychological stressors.
Because black women experience high levels of chronic stress as a result of racial discrimination, the stress hormones produced in their bodies increase their risk of adverse labor effects.
Many black women report not feeling listened to by their white doctors, especially in comparison to medical professionals of other ethnicities. For example, take Kennetha Gaines’s experience, a clinical nurse manager for the UCSF Health System in San Francisco.
Ms. Gaines was urged to have a cesarean section (c-section) for her first child after being in labor for a while and dilating to six centimeters (cm). Her doctor was white. For her second child, she switched to a Latina doctor. She wanted to try a vaginal birth after a cesarean section (VBAC), and she had the full support of her doctor. All in all, she ended up having a c-section for her second child, but she reports that the experience was very different because she “felt like [her] physician actually listened to [her].”
When doctors fail to listen to their patients sincerely, birth injuries can easily result.
Addressing the Issue
The CDC states that there are many contributing factors to pregnancy-related mortality rates. In order to address these issues, the CDC recommends “robust, comprehensive data collection and analysis through state and local maternal review committees, which thoroughly review pregnancy-related deaths and make actionable prevention recommendations.”
If you or someone you love has suffered a birth injury or mortality as a result of a medical professional’s negligence, you may be entitled to compensation. Let our skilled team see if we can help you recover it.
Contact the medical malpractice attorneys at Garau Germano, P.C. today by calling 317-978-9973 to discuss your case’s details.
